A percutaneous coronary intervention (PCI) is a minimally invasive procedure used to treat narrowed or blocked coronary arteries. When coronary arteries become narrowed by fatty deposits (atherosclerosis), blood flow to the heart can be reduced, causing chest pain (angina) or leading to a heart attack. PCI allows us to restore blood flow without the need for open-heart bypass surgery.
Angioplasty and Stenting
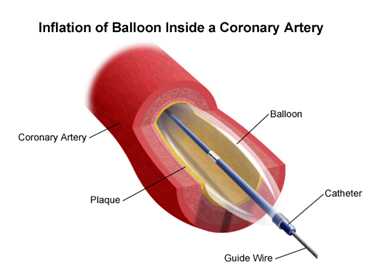
If diagnostic angiography reveals significant blockages, angioplasty can often be performed during the same procedure. A small balloon at the tip of the catheter is inflated to compress the plaque tissue (usually fatty material or clot) against the artery wall, opening the vessel. In most cases, a stent (a small mesh tube) is placed to keep the artery open.
Modern drug-eluting stents are coated with medication that helps prevent the artery from narrowing again (restenosis). These stents have significantly improved long-term outcomes for patients.
Complex and High-Risk PCI
Some patients have coronary disease that is more challenging to treat, including:
- Blockages in multiple vessels
- Disease at the origin of major arteries (left main disease)
- Heavily calcified arteries
- Chronic total occlusions (completely blocked arteries)
- Patients with other medical conditions that increase procedural risk
Our interventional cardiologists have advanced training in techniques for treating complex coronary disease, including rotational atherectomy/intravascular lithotripsy for calcified arteries, intravascular imaging guidance, and physiological assessment of blockages.
Alcohol Septal Ablation
Alcohol septal ablation is a catheter-based treatment for hypertrophic obstructive cardiomyopathy (HOCM), a condition in which the heart muscle – particularly the septum between the ventricles – becomes abnormally thickened. In some patients, this thickening obstructs blood flow out of the heart, causing symptoms such as breathlessness, chest pain, and fainting.
During the procedure, a small amount of pure alcohol is injected through a catheter into the septal artery – a small branch of the coronary arteries that supplies the thickened portion of the septum. The alcohol causes a controlled, localised injury to this area of muscle, which subsequently thins over time. This reduces the obstruction to blood flow and alleviates symptoms.
Alcohol septal ablation offers an alternative to surgical myectomy (open-heart surgery to remove excess muscle) for suitable patients. At Central Sydney Cardiology, A/Prof Mark Adams performs alcohol septal ablation and works within a multidisciplinary team to determine the most appropriate treatment approach for each patient with HOCM.
What to Expect
Most coronary interventions are performed under local anaesthesia with sedation. You will be awake but relaxed during the procedure. Access is typically through the wrist (radial artery), which allows most patients to walk soon after the procedure and go home the same day or the following day.
Following the procedure, you will need to take blood-thinning medications as prescribed to prevent clots forming on your stent. Your cardiologist will also work with you on lifestyle modifications and medications to reduce your future cardiovascular risk.
Related: Coronary Heart Disease | Invasive Cardiac Diagnostics
